What is the Honeymoon Period in Type 2 Diabetes
The honeymoon period in type 2 diabetes is a phase that often occurs shortly after diagnosis and the initiation of treatment. It’s a period where individuals with type 2 diabetes may experience a significant reduction in their blood glucose levels, sometimes even to near-normal levels. This can lead to a decrease in the need for medication, and a feeling of improved well-being. It is crucial to understand this phase as it can be both encouraging and potentially misleading if not managed properly. Recognizing the honeymoon phase and understanding its characteristics is a critical step in long-term diabetes management, as it sets the stage for proactive health strategies and sustained control of the condition.
Understanding the Honeymoon Phase
The honeymoon phase is primarily characterized by improved insulin sensitivity and, in some cases, increased insulin production by the pancreas. After diagnosis and initial treatment, which often involves lifestyle changes and medication, the body’s cells become more responsive to insulin. This means that insulin, either produced by the body or administered through medication, can more effectively transport glucose from the bloodstream into cells for energy. Consequently, blood glucose levels decrease. Lifestyle modifications such as diet and exercise play a significant role, contributing to better glucose control and a temporary respite from the more aggressive symptoms of diabetes. This period can be a valuable opportunity to reinforce healthy habits and provide a foundation for long-term management of diabetes.
Duration of the Honeymoon Period
The duration of the honeymoon period varies significantly from person to person. It can range from a few weeks to several months, and in some cases, even a couple of years. Several factors influence the length of this phase, including the individual’s age, overall health, the severity of their diabetes at diagnosis, and their adherence to treatment plans. Some individuals may experience a shorter honeymoon phase due to more advanced disease progression at the time of diagnosis, while others, particularly those who make immediate and significant lifestyle changes, may enjoy a more extended period of relatively stable blood glucose levels. Monitoring blood glucose regularly and working closely with a healthcare provider are essential to track this phase and adjust treatment as needed, as the honeymoon phase naturally progresses.
Symptoms of the Honeymoon Period
During the honeymoon phase, individuals with type 2 diabetes often experience a marked improvement in their overall health and well-being. Common symptoms that may improve or disappear include reduced thirst, decreased frequency of urination, and less fatigue. Blood glucose levels are typically closer to normal, leading to fewer instances of hyperglycemia (high blood sugar) and its associated symptoms. Many individuals also report increased energy levels and a general sense of better health. It is essential to remain vigilant during this period, as the body’s improved condition can sometimes lead to a false sense of security, making it easier to neglect the ongoing management of diabetes. Regular monitoring, adherence to treatment plans, and open communication with healthcare providers are crucial to sustaining these positive effects.
Top 7 Facts About Diabetes Type 2 Honeymoon
Fact 1 Initial Diagnosis and Treatment
The honeymoon period usually starts shortly after the initial diagnosis of type 2 diabetes and the commencement of treatment. This treatment typically includes a combination of lifestyle changes, such as diet and exercise, and, in many cases, medication to manage blood sugar levels. The immediate impact of these interventions can be profound, often leading to noticeable improvements in blood glucose control within weeks or months. It is a critical time for patients to learn about their condition and establish healthy habits. Proper education, early intervention, and adherence to medical advice during this phase are essential for maximizing the benefits of the honeymoon period and setting the stage for long-term success in diabetes management.
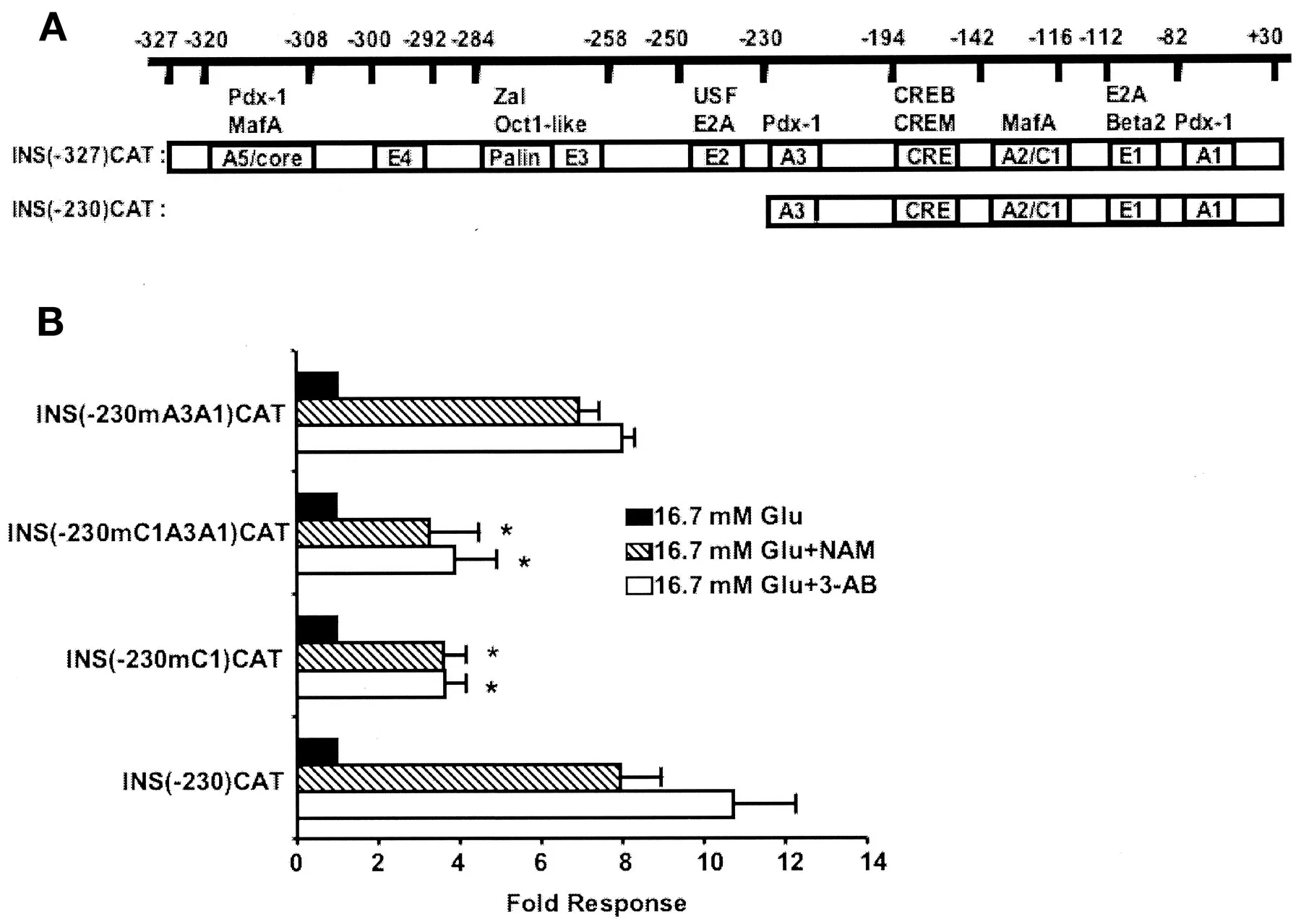
Fact 2 Improved Insulin Sensitivity
One of the primary reasons for the honeymoon period is the enhanced insulin sensitivity. Lifestyle modifications like regular physical activity and a balanced diet help improve the body’s ability to use insulin effectively. When cells become more responsive to insulin, glucose can enter them more easily, reducing blood sugar levels. This improvement is often noticeable in the early stages of treatment, as the body starts to regain its ability to process glucose efficiently. Monitoring insulin sensitivity through regular blood glucose tests and consulting with a healthcare provider can provide valuable insights into the effectiveness of the treatment plan and help make necessary adjustments to maintain optimal metabolic control.
Fact 3 Reduced Medication Needs
During the honeymoon phase, many individuals find they need lower doses of diabetes medications or even a temporary reduction in their medication regimen. Because blood sugar levels are better controlled through lifestyle changes and improved insulin sensitivity, the need for high doses of medication may decrease. This can be a welcome development for patients, as it may reduce the potential for side effects associated with medication. However, it is crucial that any adjustments to medication are made under the guidance of a healthcare professional. Regular monitoring of blood glucose levels and close collaboration with a physician are necessary to ensure that medication adjustments are safe and effective.
Fact 4 Lifestyle Impact
Lifestyle changes play a pivotal role in initiating and extending the honeymoon period. A balanced diet, rich in fiber, whole grains, and lean proteins, helps regulate blood sugar levels and supports overall health. Regular physical activity, such as brisk walking, swimming, or cycling, improves insulin sensitivity and helps the body use glucose more efficiently. These changes not only aid in the immediate management of blood sugar but also contribute to long-term health benefits, such as weight management and cardiovascular health. Sustaining these lifestyle changes is essential to maximizing the duration and benefits of the honeymoon phase, and they form a critical foundation for long-term diabetes management.
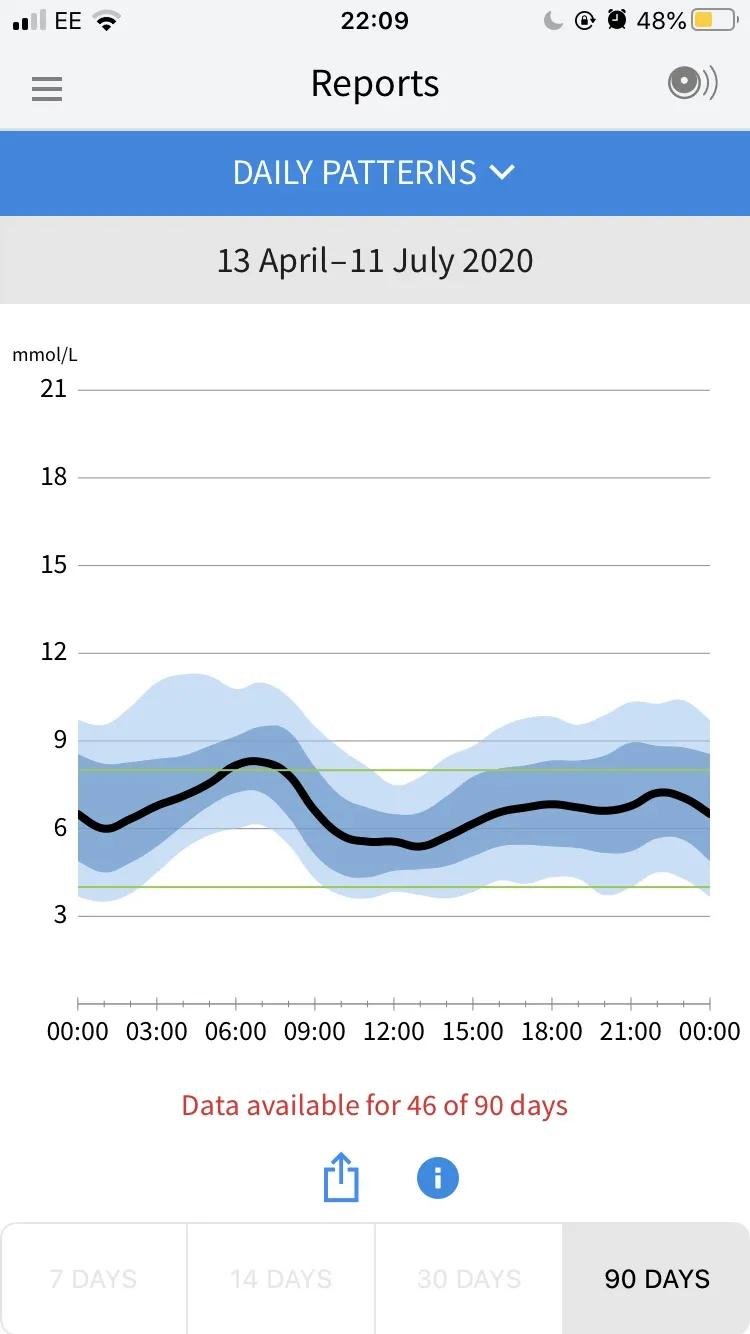
Fact 5 Importance of Monitoring
Consistent blood glucose monitoring is crucial during the honeymoon phase. Regular testing provides valuable insights into how diet, exercise, and medication affect blood sugar levels. By tracking these levels, individuals can make informed decisions about their daily routines and treatment plans. Monitoring also helps detect early signs of declining insulin sensitivity or changes in blood sugar control, enabling prompt intervention. Healthcare providers often recommend specific testing schedules tailored to individual needs, emphasizing the importance of consistent monitoring to maintain the benefits of the honeymoon period. Keeping a detailed log of blood glucose readings and sharing this information with a healthcare team is an important step in diabetes management.
Fact 6 Emotional and Psychological Aspects
The honeymoon period can have a significant emotional and psychological impact on individuals with type 2 diabetes. The improvement in blood sugar control and overall well-being can lead to increased motivation and a sense of empowerment. This is a crucial time to build positive habits and adopt a proactive approach to managing the condition. However, it’s also important to acknowledge that the honeymoon period is temporary, and as the condition progresses, the need for medication may increase. It is essential to prepare for the potential decline in blood sugar control and to continue practicing healthy lifestyle choices and adhering to treatment plans, even after the honeymoon phase ends.
Fact 7 Progression to Full Diabetes

The honeymoon period is, unfortunately, not a permanent state. As type 2 diabetes progresses, the body’s ability to produce or effectively use insulin typically declines. This means that over time, the need for medication often increases, and the blood sugar levels may become more difficult to control. Understanding this natural progression is important to managing expectations and maintaining a realistic approach to diabetes management. Regular check-ups, consistent monitoring, and adjustments to treatment plans are essential to address the evolving needs of individuals with type 2 diabetes. The key is to view the honeymoon phase as a valuable opportunity to build a solid foundation for managing the condition for the long term, accepting that the disease will evolve over time.
Tips for Managing Diabetes Type 2 During the Honeymoon Phase
Tip 1 Healthy Eating Habits
Adopting a balanced diet is crucial during the honeymoon phase. This means focusing on nutrient-rich foods that help regulate blood sugar levels. Prioritize foods with a low glycemic index (GI), such as non-starchy vegetables, whole grains, lean proteins, and healthy fats. Limiting processed foods, sugary drinks, and excessive carbohydrates helps to maintain stable blood sugar levels. Portion control is another important aspect of healthy eating, as it ensures that you consume the right amount of calories and nutrients. Eating regular meals and snacks throughout the day can also help to prevent blood sugar spikes and keep energy levels consistent. Consistent healthy eating habits during this phase set a strong foundation for long-term diabetes management.
Tip 2 Regular Physical Activity

Engaging in regular physical activity is a cornerstone of diabetes management during the honeymoon phase. Exercise increases insulin sensitivity, which allows the body to use insulin more effectively and lowers blood sugar levels. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, swimming, or cycling. In addition to aerobic exercise, incorporate strength training exercises at least two times per week to build muscle mass, which helps improve glucose control. Physical activity not only helps manage blood sugar but also contributes to weight management, improves cardiovascular health, and boosts overall well-being. Finding enjoyable activities and integrating them into your daily routine makes exercise more sustainable and beneficial.
Tip 3 Blood Glucose Monitoring
Consistent blood glucose monitoring is essential during the honeymoon phase to track how lifestyle changes and medication are affecting blood sugar levels. Regular testing allows you to identify patterns and trends, which helps you make informed decisions about your diet, exercise, and medication. Follow the monitoring schedule recommended by your healthcare provider and keep a detailed log of your readings. This log should include the date, time, blood sugar level, and any factors that may have influenced the reading, such as food intake or exercise. Sharing this information with your healthcare team during regular check-ups helps them adjust your treatment plan as needed and ensure that you are maintaining optimal blood sugar control. A blood glucose monitor is a vital tool to effectively manage your condition.
Tip 4 Medication Adherence
If you’ve been prescribed medication for type 2 diabetes, adhering to the prescribed dosage and schedule is crucial during the honeymoon phase. Even if you experience improved blood sugar control, continue taking your medication as directed unless your healthcare provider instructs you otherwise. Never adjust your medication without consulting your doctor, as this could disrupt your blood sugar management. Adhering to your medication plan ensures that you maintain the benefits of the honeymoon phase and prevents blood sugar levels from rising again. If you have any concerns or experience side effects from your medication, discuss them with your healthcare provider promptly. Medication adherence is an essential part of maintaining control over type 2 diabetes.
Tip 5 Regular Check-ups
Regular check-ups with your healthcare provider are vital during the honeymoon phase. These visits allow your doctor to monitor your overall health, review your blood glucose readings, and assess the effectiveness of your treatment plan. During check-ups, your doctor can also identify any potential complications, such as kidney or eye problems, and provide guidance on how to manage them. Discuss any changes in your symptoms or medications with your doctor and ask questions about your health. These check-ups provide an opportunity to ensure your diabetes management strategy remains effective and appropriate. Regular check-ups are an essential investment in your health and well-being, offering a supportive partnership with your healthcare team.
Tip 6 Stress Management
Managing stress is crucial during the honeymoon phase, as chronic stress can negatively affect blood sugar levels. Find healthy ways to cope with stress, such as practicing relaxation techniques, deep breathing exercises, or meditation. Regular physical activity, like yoga or tai chi, can also help reduce stress levels. Make time for activities you enjoy, such as hobbies or spending time with loved ones. If you find that stress is overwhelming, consider seeking support from a therapist or counselor. By prioritizing stress management, you can maintain better blood sugar control and improve your overall well-being. Stress management is an important part of a comprehensive approach to diabetes care.
Tip 7 Education and Support
Continuing your diabetes education and seeking support from others is crucial during the honeymoon phase. Learn as much as you can about type 2 diabetes, its management, and potential complications. Attend diabetes education classes, workshops, or online resources to expand your knowledge and skills. Join a diabetes support group or connect with other individuals with diabetes to share experiences, exchange tips, and receive emotional support. Support groups can provide valuable insights and help you feel less alone in your journey. Education and support empower you to take an active role in managing your diabetes and maintaining your health. Staying informed and connected will help you navigate the honeymoon phase and beyond.
Long-Term Outlook and Management of Diabetes Type 2
Preventing Complications
Preventing complications is a central focus in the long-term management of type 2 diabetes. This involves consistent efforts to keep blood sugar levels within a target range, as well as regular check-ups and screenings to detect any early signs of complications. By taking proactive measures, such as following a healthy diet, engaging in regular physical activity, and taking medications as prescribed, you can significantly reduce the risk of developing serious complications. Also, regular check-ups with your healthcare team and a proactive approach to your health are paramount in mitigating long-term complications. Preventing complications allows you to live a full and healthy life.
Importance of Continuous Care
Managing type 2 diabetes is a lifelong commitment, and continuous care is essential for maintaining good health. This includes regular visits with your healthcare team, adherence to your treatment plan, and ongoing self-monitoring of blood sugar levels. Continuous care also involves staying informed about the latest advances in diabetes management and being proactive in addressing any concerns or issues that arise. By making diabetes management an ongoing priority, you can enjoy a better quality of life and minimize the impact of diabetes on your overall health. The cornerstone of the treatment is a strong relationship with your healthcare provider, and consistent adherence to your treatment.
